IMPORT
High driving nipple deformation is not an unusual complication after masticity, breast reconstruction or breast reconstruction after nipple mastectomy. In a study that included 18 patients receiving mastectomy and reconstruction of the irradiated breast, 55.6% of patients suffered from high-level nipple complications after 3 years[1]. Eight-two international publications on breast breasts and reductions were analyzed by Swanson[2] And the result showed that 41.9% of patients had at least one excessive nipple. Procedures that use marginal incisions inhibit a large amount of skin, which results in high -driving nipple, areola expansion and hypertrophic scars[3,4].
Reduction of high driving nipple has always been a main challenge for breast surgeons due to the insufficient availability of the skin between the cellar and the nipple. There was a limited number of techniques. The reported approaches include an increase in reception decimal[5]mutual wings[6]Z-Plasty fin[7]and reinstalled graft[8]. However, these techniques are unable to shrink the enlarged area. The upper pole area is the exposed area of attraction of the female, and females have no intention of leaving any rose and surgical scars in this area, indicating that the decrease in high -riding nipple is not enough, and the need to reduce the diameter.
This report describes a case of correction of high -driving nipple deformation with the enlarged area after breast mastics, which has shown a new strategy for similar cases. The extension of the tissue of the upper pole of the breast was applied to achieve free tension around the environment rotary suture when the size of the area was reduced. This technique suggested a feasible therapeutic option for severe postoperative elevation and area expansion.
Presentation
Head of complaints and a history of illness
A 26 -year -old woman, who previously underwent breast companies, was accepted to our hospital and requested correction for high -driving nipple with enlarged area. She underwent Mammoplasty Augmentation 5 years before her admission to our hospital. Two months before she entered our hospital, only Mastopexy took place. However, she was still unhappy with her chest and underwent 1 MO fat cuttings before she was accepted. All of these surgeries were performed in other institutions. These surgeries also aim to raise breasts and nipples, while the nipples were incorrectly placed very high, which resulted in an unnatural shape accompanied by a breast wing (shape 1a).
Figure 1 preoperative and photo monitoring.
A: Preoperative photo. B: Three months after the first stage. Each dilator was filled at 350 ml. C: Three months after the second stage. The design of Mastopexy surgery. D: Monitoring one year after the third stage.
Examination
The left and right -diameters Areola were 9 and 8 cm, respectively, including the staining lip. PERI-AROLA has obvious hypertrophic scars and the decline has not improved. According to the most detailed classification system presented by Scott et al[9]The patient’s nipple was at 36th percentage of vertical breast height (figure 2). Were ranked as a shift of the Nipple-AROLA Complex (NAC) complex, which showed the elevated nipple to 45th to 35th centimeter.
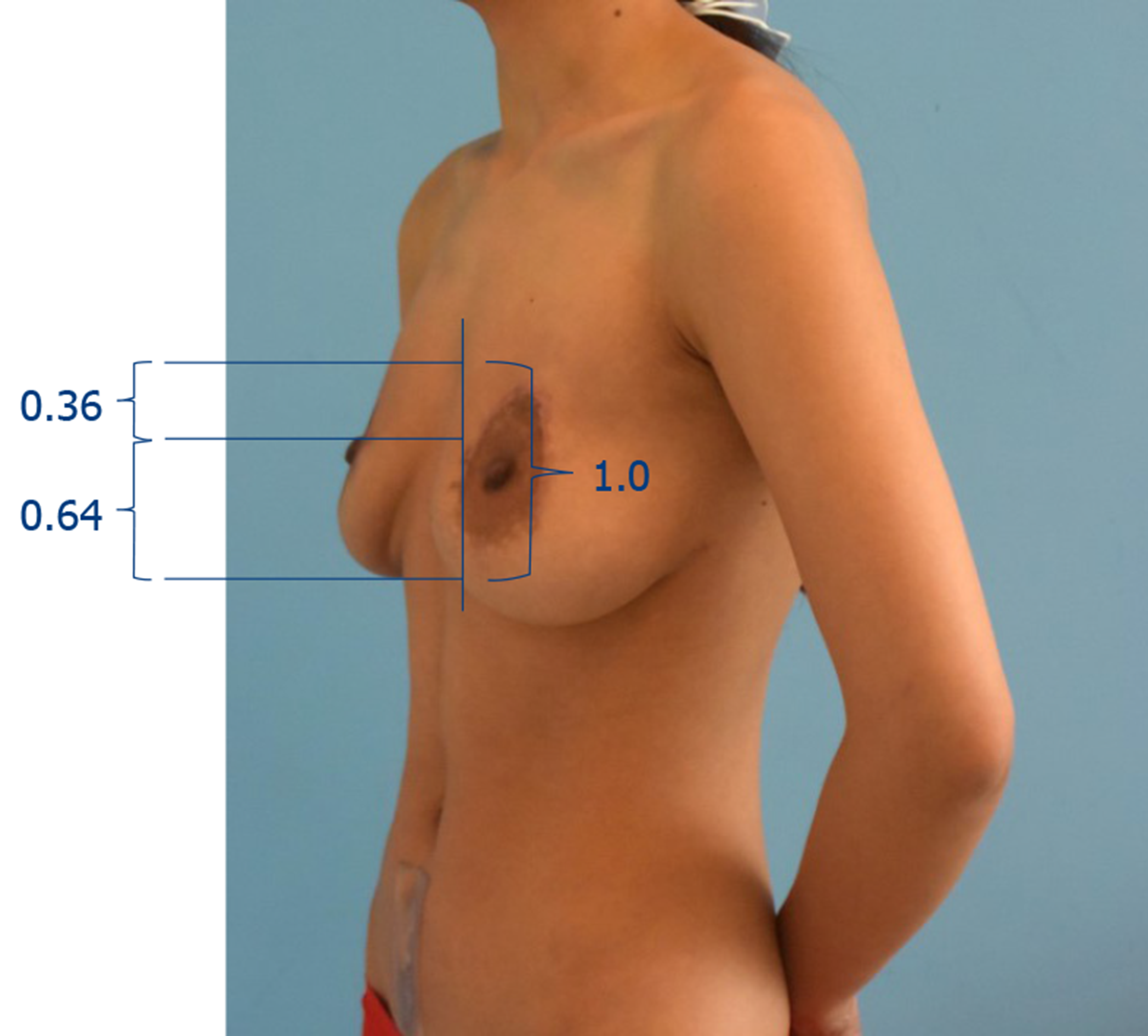
Figure 2 preoperative oblique view.
The patient was classified to have a mild nipple-abeola complex shift.
Final diagnosis
The final diagnosis of the presented case was the high quality nipple with enlarged area.
TREATMENT
After understanding the risks and benefits of the surgery of review, consent from the patient was received. Prior to surgery, the distances of the ultrasound to the nipple were 17.5 cm on the right and 17 cm to the left, respectively. In the first stage, 300 cc kidney tissue extensions were placed in the subcutaneous space in the upper pole to expand more skin, increasing the absolute distance from the notch to nipple. We made the cut along the upper line of Areola where the old scars were. Each dilator was filled with a total of 350 ml of saline water over a period of 3 MO (shape 1b). In the second stage, the exploitation was removed through the same incision and pocket (Supplementary Figure 1). The ribs of ribs were used to avoid withdrawal of extensive skin. Three months after it was accepted in our hospital, when the skin stopped the contraction and the nipple notches reduced to 19 cm on both sides, the third stage of the revision review was taken. When the patient was upright, preoperative skin signal took place taking into account the desired nipple position, blood supply and minimum scars (shape 1C). The incision combines modified round pattern with an inverted T-Incision pattern. The vascularity in the nipple-aveola complex was based on the lower pedicle. Intraoperatively, Araola was at maximum intensity in a diameter of 40 mm. The marginal and vertical departments of degraded and the vertical section are engaged through a sub-section. We removed the directed tissue and construction of structure with the side and medium pillars (Supplementary shapes 2 and 3). Peripheral and vertical incisions were closed with a 3-0 monodermi device and intraodermal monocryl stitches to reduce the subsequent adverse scars.
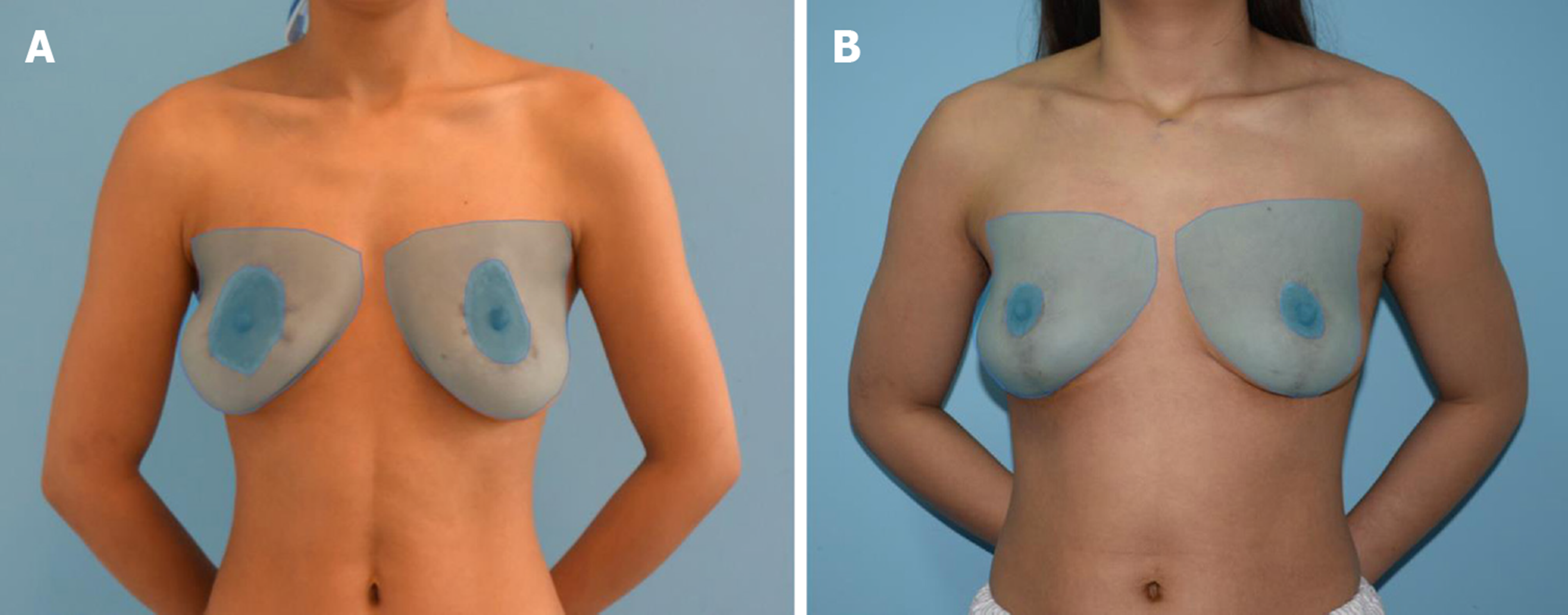
Figure 3 The ratio of the nipple-mara and entire breast area.
A: The preoperative area proportions left and right were 23.5% and 16.5% respectively. B: Postoperative area proportions left and right were 5.1% and 5.4% respectively.
Result and monitoring
The patient did not show a postoperative complication. After 1 year of admission, both of the Areola diameters were measured at 4 cm and mounted symmetrically. Most importantly, the patient was satisfied with breast outline (figure 1D).
DISCUSSION
High -driving postoperative nipple with enlarged area is an aesthetically devastating problem for patients and is also a huge challenge for plastic surgeons. When the high -driving nipple is combined with the fall, it becomes even more difficult to process because traditional mastics can increase the position of the nipple after surgery. In this test, the patient underwent several breast companies before the revision of Mastopexy. The goals of this case included a decrease in the nipple, the reduction of the size of ARola, to ensure the supply of nipple blood and the improvement of volatile breast poetry. We have demonstrated the successful use of the holding in conjunction with Mastopexy to repair the high driving nipple with the enlarged nipple-AROLA complex.
The extensions were placed via The existing old scars around the area. The increased distance from the notch-gentle before the masticon was aimed at avoiding the increased nipple after masticity, which can make the nipple to be overly high to hide in the bra. At the same time, the increased distance from the notch to a nipple can provide additional space to correct the enlarged area. In addition, meticulous dissection is an important step in maintaining blood supply. The marginal incision standard and the inverted T-INCISION standard could minimize the length of the scar. Although this technique requires multi -stage processes, it can successfully improve the appearance of breasts.
However, the breasts appeared flat one year after the final procedure due to the lack of adequate parenchyma tissue. Another breast increase technique (such as the implantation process) could achieve a superior appearance, however, the patient has already been satisfied and this technique was not used. Cylinder et al[10] It presented a similar technique to reduce the high driving nipple and only the dilator could have a satisfactory outline of the breast. In this case, the enlarged area made it more complicated and we needed to combine modified round block pattern with inverted T-Incision pattern to correct deformation. Therefore, further study should be carried out to achieve the appropriate spaces between procedures, making the balance of skin contraction and the duration of treatment.
The most reliable sorting of the high-driving nipples-aROLA complex is based on the position of the nipple along the vertical axis of the breast[9]. According to this sorting system, this case was classified as a mild NAC displacement. However, we believe that the aforementioned classification is not reasonable when there is a great feast. The NAC and Breast Area was marked in preoperative and postoperative photos (figure 3). Imagej software was used and the percentages of the preoperative areas left and right breast were 23.5% and 16.5% respectively. However, these postoperative rates decreased to 5.1% and 5.4%, respectively, indicating the natural and reasonable size of the nipple.
CONCLUSION
In summary, this case has proposed a feasible method for processing the high driving nipple with enlarged area and can be used in other similar cases. In addition, with regard to the size of the area, a new high -driving NAC sorting system is necessary to further help clinicians to design an effective surgical plan.
Handwriting: Unwanted manuscript
Specialist: Medicine, Research and Experimental
Country/territory of origin: China
The scientific quality classification of review by peer
Grade A (excellent): 0
Grade B (very good): B, b
Grade C (good): 0
Grade D (fair): 0
Grade E (poor): 0
P-Reviewer: Vaudo g, ziogas de S-Editor: Wang jl L-Editor: Wang TQ E-Editor: Liu Jh

