When a pathogen invades the body, it can cause significant damage on its own. But just as often, the real destruction can come from the body’s own defenses. This applies to periodontal disease, also known as gum disease, as it refers to the inflammation of the gums surrounding the teeth. Periodontal disease often begins with the growth of sticky films of bacteria that later lead to chronic gum inflammation, bone loss, and sometimes tooth loss.
A new treatment that delivers a protein that modulates the host’s local immune response could help treat this condition, according to a recent study. Researchers led by Charles Sphere at the University of Pittsburgh School of Dentistry reported that the injection of microparticles loaded with this immunomodulator into a mouse model of periodontal disease inhibited bone loss and accelerated recovery at different stages of the disease (1).
While current interventions such as deep cleaning, antibiotics and surgery can help patients with periodontal disease, they come with limitations. For example, repeated use of antibiotics can contribute to the development of antibiotic resistance. “It’s not like you can give someone chronic antibiotics for the rest of their life to treat periodontal disease,” he said. Yvonne Hernandez-Capilaclinical scientist at the University of California, Los Angeles, who was not involved in the new work. Because of these limitations and the variability in patient response to treatments, there is always a need to seek alternative treatments, he added.
It’s not like you can give someone chronic antibiotics for the rest of their life to treat periodontal disease.
– Yvonne Hernandez-Kapila, University of California, Los Angeles
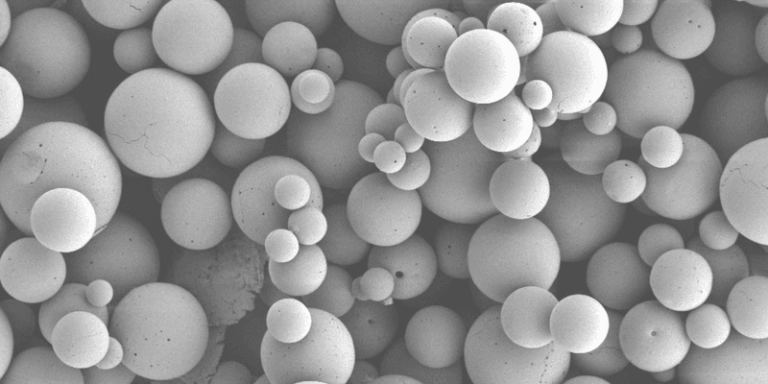
Unlike most existing interventions for gum disease that primarily target the bacteria that cause the condition, Sfeir and his team focused on modulating the immune response, which is key to the development of periodontal disease. They constructed microparticles containing the CC motif of chemokine ligand 2 (CCL2), a protein that under certain conditions causes a macrophage response which promotes resolution of inflammation and tissue repair (2,3). These microparticles are encapsulated in a degradable polymer, allowing gradual and sustained release of CCL2 for at least 30 days after delivery.
The team then induced periodontal disease in mice by placing a silk ligature around a tooth to promote plaque biofilm build-up. To test the effect of the treatment as a preventive, interventional, or restorative approach, respectively, they injected mice with CCL2 microparticles at one of three stages: the day of ligature placement, four days later, or the day of ligature removal. The treatment reduced bone loss by 32 to 37 percent in the prevention group and 26 to 29 percent in the intervention group, compared with control mice (which were either untreated or treated with microparticles without CCL2). Mice given CCL2 after the ligation was removed regained up to 56 percent of bone, compared with 17 to 30 percent in the control groups.
These results resulted primarily from the ability of CCL2 to promote an anti-inflammatory phenotype in macrophages. Specifically, single-cell RNA-sequencing analyzes of immune cells in the gums of treated mice revealed that CCL2 treatment inhibited myeloid cell-expressed activating receptor-1 (TREM-1), which causes periodontal inflammationwhile activating protein kinase A (PKA), involved in resolution of inflammation (4,5). In addition, CCL2 indirectly affected the presence of bacteria around the tooth, reducing the bacterial load in the area, likely reducing nutrients derived from tissue destruction.
Hernandez-Kapila said Sfeir and his team showed strong evidence that CCL2 microparticles prevented bone loss in this ligation-induced mouse model of periodontal disease. However, “[this] it’s a very acute and aggressive model of the disease,” he said, indicating that the model does not accurately represent the chronic nature of the condition. “No model is perfect,” he acknowledged, and emphasized the importance of testing the treatment in animal models of other periodontal diseases before translating it to humans. He also stressed the need to assess any toxic effects of the drug — for example, by examining the livers and kidneys of treated mice. Despite the local tradition, he noted, it’s unclear whether the agent could be incorporated into the bloodstream, especially since oozing gums are a hallmark of periodontal disease.
Sfeir said his team has tested the treatment in another mouse model and in dogs, but those results have not yet been published. Regarding toxicity, he explained that since the microparticle content is released at the nanogram level, it will be difficult to detect in tissues. “What we did very early on was feed the mice milligrams of microparticles, and we didn’t see any toxicity,” he said. As the team prepares for a submission to the Food and Drug Administration (FDA), Sfeir noted that they will likely conduct these toxicity studies according to specific guidelines. “We don’t expect to see any toxicity because of the small amounts that are released,” he said.
Overall, the results so far are exciting, Hernandez-Kapila concluded. Since “it’s a new thing for us to try, it gives hope,” he said.
References
- Shehabeldin, M. et al. Therapeutic administration of CCL2 modulates the immune response and restores host-microbe homeostasis. Proc Natl Acad Sci 121e2400528121 (2024).
- Wood, S. et al. The proinflammatory chemokine CCL2 (MCP-1) promotes healing in diabetic wounds by restoring the macrophage response. PLoS One 9e91574 (2014).
- Roca, H. et al. CCL2 and interleukin-6 promote survival of human CD11b+ Peripheral blood mononuclear cells and induce M2-type macrophage polarization. J Biol Chem 28434342-54 (2009).
- Wu, D. et al. Trem1 induces periodontal inflammation through regulation of M1 polarization. J Dent Res 101437-447 (2022).
- Kong, D. et al. The PKA IIα regulatory subunit is essential for PGD2– mediated resolution of inflammation. J Exp Med 2132209-26 (2016).