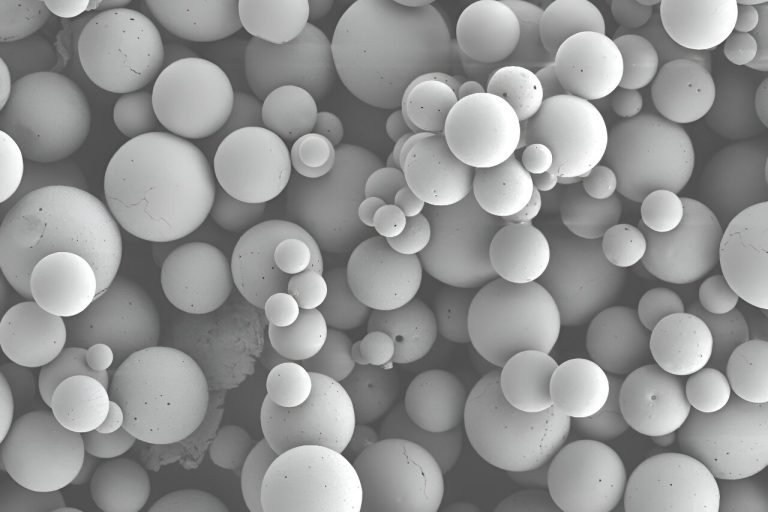
Microparticles containing the immunomodulatory compound CCL2. Credit: Julie Kobyra, University of Pittsburgh
Targeting the immune system could prevent or treat periodontal disease (PD), a common but serious gum disease, according to new research from the University of Pittsburgh.
The study, published in Proceedings of the National Academy of Sciencesshowed that delivering microparticles containing the immunomodulatory compound CCL2 directly to the gingiva inhibited bone loss and accelerated bone repair in a mouse model of PD.
“Treatment for PD has always focused on targeting bacteria, but bacteria do not cause the disease. Instead, they trigger PD by activating the immune system, which leads to inflammation and bone loss around the teeth,” said senior author Charles Sfeir , DDS , Ph.D., associate professor and chair of the Department of Periodontology and Preventive Dentistry at Pitt School of Dental Medicine and member of the McGowan Institute for Regenerative Medicine. “Our study shows that it goes both ways: If we curb the immune system, we can change the composition of the bacteria and prevent the disease from occurring or stop it from progressing.”
Sfeir collaborated with Steven Little, Ph.D, distinguished professor and chair of the Department of Chemical and Petroleum Engineering in the Swanson School of Engineering and a McGowan Fellow, who developed microparticles that provide sustained release of CCL2.
“The potential for mechanical systems to interact with the immune system of the periodontal space is huge and represents a completely different way of treating disease compared to what is done clinically now,” Little said. “This collaboration with Dr. Sphere is further proof of the exciting future for these types of technologies.”
Led by first author Mostafa Shehabeldin, MS, Ph.D., who was a graduate student in Sfeir’s lab and is now an assistant professor of periodontics at UT Health San Antonio, the researchers first induced PD in mice by tying around a thread silk. one of their molars. Silk quickly accumulates bacteria, causing inflammation that begins to rapidly destroy the bone around the teeth in as little as four days.
To see if CCL2 could prevent PD or treat active disease, the researchers treated the animals with the microparticles at the same time as silk placement or four days after. They also tested whether CCL2 would affect the self-resolving disease by treating mice with microparticles at the same time as removing the silk.
In all three scenarios, CCL2 treatment helped prevent or treat PD by reducing bone loss and improving bone repair.
This beneficial effect came from changes in macrophages, the white blood cells that kill microorganisms, remove dead cells, and stimulate other immune cells. In PD, most macrophages are of the inflammatory M1 type, but CCL2 treatment shifted them to an anti-inflammatory M2 type.
Injecting microparticles also altered the oral microbiome, reducing or preventing increases in total bacterial load and the abundance of certain bacterial species associated with PD.
“PD is a highly prevalent inflammatory disease that affects many patients to varying degrees of severity,” said Sfeir. “This research is exciting because it has the potential to impact so many people.”
According to Sfeir, who hopes to test this new approach to treating PD in a future clinical trial, CCL2 therapy will likely be developed as an adjunctive therapy that would work alongside traditional bacteria-targeting treatments that include regular dental cleanings and antimicrobials.
“For 70 to 80 percent of the PD population, they get a dental cleaning and the inflammation goes down,” Sfeir said. “But a small fraction of patients, even though they clean regularly and maintain meticulous oral hygiene, still experience bone destruction. Something like CCL2 would really help.”
The findings also offer new insights into understanding the interactions between the immune system and the microbiome.
“The oral cavity is one of the few areas of the human body where you can study interactions between microbes and the immune system, and it’s much more accessible than other areas like the gut and lungs,” Sfeir said. “This makes PD a really important model system for other immune-driven diseases.”
Other authors on the study were Jin Gao, Ph.D., Yejin Cho, Rong Chong, MS, Tracy Tabib, MS, Sarah Gaffen, Ph.D., and Robert Lafyatis, MD, all of Pitt. and Lu Li, Ph.D., Matthew Smardz, Patricia Diaz, Ph.D., DDS, all from the University at Buffalo.
More information:
Mostafa Shehabeldin et al, Therapeutic delivery of CCL2 modulates the immune response and restores host-microbe homeostasis, Proceedings of the National Academy of Sciences (2024). DOI: 10.1073/pnas.2400528121
Reference: Immunotherapy for gingivitis? Mouse study shows promise (2024 September 30) retrieved September 30, 2024 from
This document is subject to copyright. Except for any fair dealing for purposes of private study or research, no part may be reproduced without written permission. Content is provided for informational purposes only.