Lauren Kuhn Nuth presents a successful root canal retreatment case she completed using Septodont’s BioRoot Flow.
Import
The success rate of non-surgical root canal treatment is high. However, inadequate occlusion and inability to seal anatomical complexities may play a role in the long-term success of endodontic treatment.
Traditional root canal sealants tend to shrink or wash out. BioRoot Flow is a mineral-based tricalcium silicate sealant with bioactive properties, which expands slightly on setting and has a high pH, therefore providing antimicrobial properties.
Methods
The patient presented with a previously treated tooth #30 (mandibular right first molar) with apical periodontitis and non-retarded dysglossia (DL)
and medium medium (MM) channels. The case was re-treated by the author, and at one-year follow-up, excellent healing of the apex had occurred.
Discussion
Successful root canal retreatment requires eradication of bacteria from the canals and long-term sealing of the canals. The active biosilica technology in BioRoot Flow enables antimicrobial effects and top bone healing.
Conclusion
BioRoot Flow played a critical role in the success of this case’s root canal re-treatment, with excellent sealing and antimicrobial properties.
Clinical signs and symptoms
The patient presented in June 2022 for consultation. Her dentist and hygienist recently noted periapical radiographs associated with tooth 30 (mandibular right first molar) on a complete set of mouth radiographs. The patient was asymptomatic, but because she was told she might have an “infection,” she presented to the author for an endodontic examination.
The dental history was remarkable for root canal treatment of tooth 30 performed in 2016. No follow-up radiographs had been obtained since 2017.
Diagnosis
An extraoral and intraoral examination was performed. There was no lymphadenopathy, edema, erythema, or sinusitis. Tooth 30 was nontender to percussion and palpation, had normal mobility, a mid-buccal probing of 4 mm (all others were <4 mm), and was unresponsive to cold due to prior endodontic treatment. The tooth is currently restored with a porcelain fused to metal (PFM) crown with composite material in the access cavity.
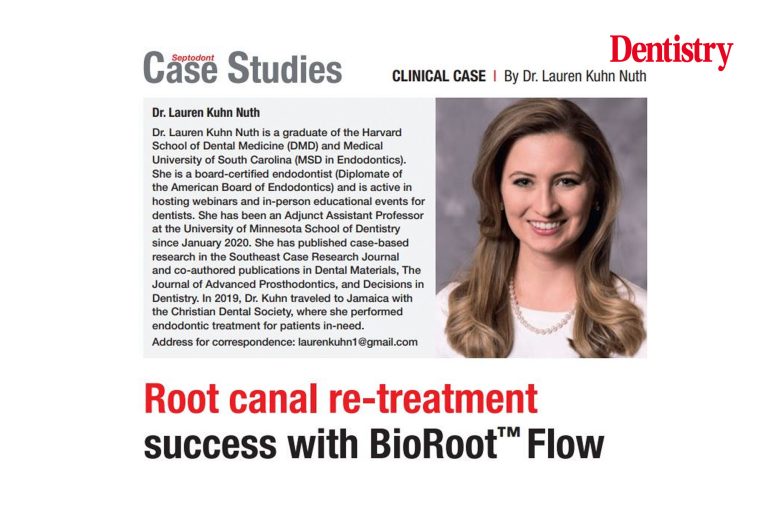
For radiographic diagnosis, a periapical (PA) radiograph (Figure 1) and limited field of view CBCT (Figures 2a-d) were performed. Previous endodontic treatment included a three-canal obturation, with insufficient obturation density in the apical 1/3 of the M and D roots. Apical radiations were present at the mid (3x3mm) and distal (3x5mm) apex.
CBCT (Figures 2a-d) confirmed an unobstructed apostolic canal (DL) and possible middle middle (MM) canal. the coronal CBCT section of the median root (Figure 2c) also suggests an apical delta, rather than a single apical foramen. No signs of cracking or fracture were visible.
Procedure and treatment
Two days after the consultation appointment, the patient presented for a non-surgical redo of the root canal of tooth 30. Informed consent was reviewed and obtained.
Local anesthetic and elastic barrier isolation were performed. The access cavity was opened to give access to the previously occluded as well as untreated channels.
Manual and rotary instruments, along with a solvent, were used to remove the existing gutta-percha in the MB, ML, and DB canals. DL and MM channels were also identified and organized. The electronic peak locator was used to determine working lengths for each channel. Passability received on all channels. The canals and chamber were irrigated with 6% NaOCl (30-gauge, side-vented needle).
Gentle wave irrigation was used as a supplement to traditional irrigation. Gutta-percha was placed in each canal and a master cone radiograph was taken to ensure proper fit. The canals were dried and BioRoot Flow sealer was injected into the middle of all canals, using the luer-lock tip provided by the manufacturer.
The tip of the BioRoot Flow syringe was then removed and the gutta-percha cones were coated by carefully inserting them into the remaining sealant at the tip of the syringe. This allows savings in sealant but also complete occlusion. Once the cones were covered, they sat lengthwise. A heated plug was used to bake the gutta-percha at the level of the mouth, followed by compression. Access was then restored.
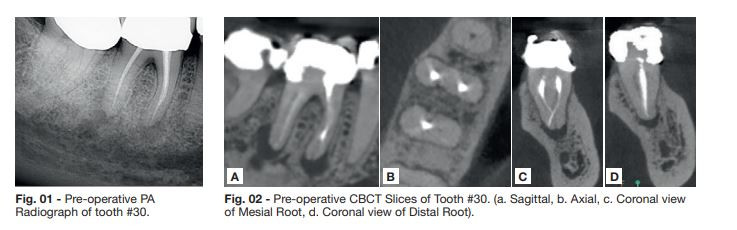
A postoperative PA radiograph was taken (Figure 3) and home care instructions were reviewed. The next day, the patient was called on the phone to see if she had any questions or concerns. He said he was doing well but was in a bit of pain and had taken ibuprofen once.
Six-month follow-up
In January 2023, the patient returned for a routine six-month follow-up appointment and stated, “I’m fine!”
Clinical examination was performed and mid-buccal probing had returned to a normal depth of <4 mm. All teeth in the quadrant were tender to percussion and palpation. There were no signs of erythema, edema, or sinus tract.
The patient consented to a PA radiograph and limited-field CBCT scan. PA radiograph (Figure 4) shows a small medial regurgitation. The apical radiations associated with the middle and distal roots have decreased in size since June 2022 (compare figure 1 and figure 4).
CBCT (Fig. 05) shows a significant reduction in the size of the apical lesions, demonstrating excellent healing at the six-month point.
Recommendation: Follow-up at six months, as healing is expected to be nearing completion at 12 months.
One year follow-up
In June 2023, the patient returned for a 12-month follow-up, stating: “I’m fine. Just here for a routine check.’
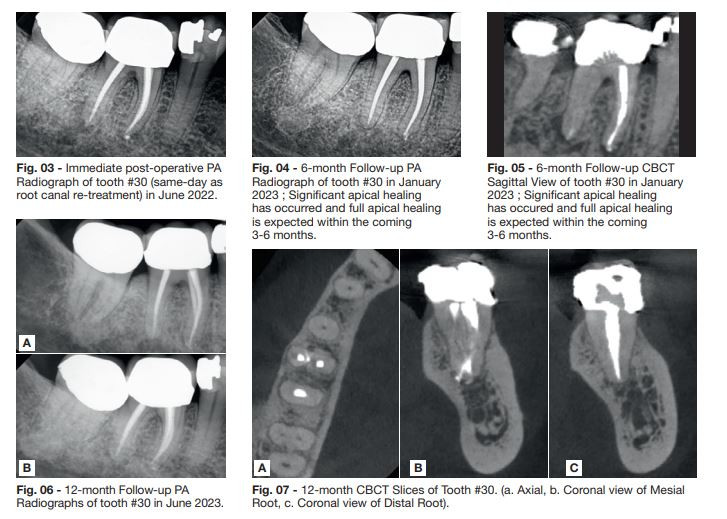
The patient is asymptomatic and probing depths were all <4mm around 30. Tooth 30 was tender to percussion and palpation, with normal mobility. The patient consented to PA radiographs (Figures 6a-b) and a limited field of view CBCT scan (Figures 7a-c). PA radiographs (Figures 6a-b) show signs of healing in both the medial and distal apex.
CBCT (Figure 7a) highlights obstruction of the middle intimal duct and convergence/union of the DB and DL ducts. Coronal views M and D (Figures 7b-c) confirm apical healing of both roots.
Clinical and radiographic findings indicate that 30 have been cured. No further follow-up is required unless the patient or her dentist notices changes in clinical or radiographic signs/symptoms.
Creating an environment for healing
The goal of endodontic treatment is to create an environment where apical periodontitis can heal. Studies show that “failure in endodontic treatments is related to the poor quality of root canal sealings” (Marconi et al, 2022). Many clinicians wish to improve their obturation techniques as this can minimize the chance of failure and reinfection.
A 2022 systematic review found that “there are no differences in the success rate of primary non-surgical endodontic treatments when the cold lateral condensation technique and other occlusion techniques are performed. Further well-designed studies are still necessary’ (Marconi et al, 2022). Therefore, clinicians can choose from a variety of occlusion techniques and can choose the technique that works best in their hands.
In this case study, a monocone/hydraulic compaction technique was used. This technique is generally considered a “cold” technique since heat is applied only at the level of the mouth to remove excess gutta-percha. Cold techniques are mandatory with some sealants, as the application of heat can alter the setting process of the sealant. This is not the case with BioRoot Flow, as the sealant is fixed in the canal using the inherent moisture and moisture of the root dentin. This means that all hot and cold techniques are acceptable for use with this sealant.
Antimicrobial treatment
Furthermore, it is known that approximately 35% of the root canal walls are not touched by endodontic instruments (Peters et al, 2001). This means that endodontic success relies on a combination of antimicrobial treatments (such as fluids and sealants) and obturation to minimize the space where bacteria can survive and multiply.
BioRoot Flow is extremely pure and biocompatible. This allowed the small puff in the middle of the case to be well received by the body. Additionally, BioRoot Flow expands slightly upon setting, which helps block the dentinal tubules where bacteria can survive and multiply. Finally, the high pH of the sealer contributed to the provider/author’s antimicrobial efforts.
BioRoot Flow builds on the legacy of BioRoot RCS, which was introduced in 2016. BioRoot Flow became available in 2022, making activated biosilicate technology easier to use in a syringeable form. Studies show that calcium silicate-based sealants promote apical healing, are antibacterial, and bond to tooth structure. Their biological properties depend on… a hydration reaction followed by a calcium phosphate precipitation reaction and hydroxyapatite formation” (Zavattini et al, 2020). These properties have enabled clinicians to achieve high quality endodontic results for their patients.
Conclusion
Septodont’s BioRoot Flow builds on the legacy of BioRoot RCS, which is known to be non-cytotoxic and induce angiogenesis and osteogenic growth (Camps et al, 2015). In this case study, BioRoot Flow played a critical role in the success of the root canal re-treatment, with excellent sealing and antimicrobial properties.
References
- Camps, Jean et al. Bioactivity of calcium silicate-based endodontic cement (BioRoot RCS): Interactions with human periodontal ligament cells in vitro. Journal of EndodonticsVolume 41, Issue 9, 1469 – 1473 (2015).
- Marconi DF, da Silva GS, Weissheimer T, Silva IA, Só GB, Jahnke LT, Skupien JA, Só MVR, da Rosa RA. Effect of root canal filling technique on the success rate of primary endodontic treatments: a systematic review. Restor Dent Endod. 2022 Oct 11, 47(4):e40. doi:10.5395/rde.2022.47.e40. PMID: 36518607; PMCID: PMC9715375 (2022).
- Peters, OA, et al. (2001). Effects of four Ni-Ti preparation techniques on root canal geometry assessed by micro-computed tomography. Int Endod J34(3), 221–230.
- Zavattini A, Knight A, Foschi F, Mannocci F. Outcome of root canal treatments using a new calcium silicate root canal sealer: A non-randomized clinical trial. J Clin Med. 2020 Mar 13;9(3):782. doi: 10.3390/jcm9030782. PMID: 32183124; PMCID: PMC7141324.
For more information on BioRoot Flow, visit www.septodont.com.
This article is sponsored by Septodont.