Most plastic surgeons experienced with UAL have reported better results with less fatigue in the treatment of fibrous areas such as gynecomastia,
[6] the back, upper abdomen and rear hip rolls (see images below).
[7] Areas with less dense fat such as the inner knee and inner thigh generally do not benefit from the application of ultrasound with lipoplasty. UAL is an adjunct to lipoplasty rather than an alternative methodology.
Patient 1 before ultrasound-assisted liposuction (used with permission from Baxter Plastic Surgery).

Patient 1 after ultrasound liposuction (used with permission from Baxter Plastic Surgery).

Patient 2 before ultrasound liposuction (used with permission from Baxter Plastic Surgery).

Patient 2 after ultrasound liposuction (used with permission from Baxter Plastic Surgery).
Second-generation devices (eg, Lysonix, Mentor) use hollow cannulas for simultaneous aspiration and ultrasound delivery, allowing monitoring of aspiration quality. When the suction changes from pale yellow to pink or gray, emulsification is complete. This is a clinically important endpoint that should be observed when using second-generation devices.
Second generation devices also have some disadvantages. They are relatively large in diameter (≥5 mm), which requires larger incisions to accommodate skin shields. The lumen is small, resulting in insufficient suction. Therefore, a 2-stage process is generally performed with a second suction-only component. Furthermore, the ultrasound energy is focused in a longitudinal direction, just away from the edge. this may increase the risk of burns.
The third generation technology returns to the solid probe with some changes in the probe design (vibration amplification of sound energy in resonance [VASER]Sound Surgical Technologies LLC, Louisville, Colo).
[8, 9] Grooves in the probe near the tip result in radial dispersion of acoustic energy, yielding more efficient emulsification with lower total energy application. These probes are 2.9 mm and 3.7 mm in diameter, so smaller incisions are required. Some evidence suggests that VASER liposuction reduces blood loss compared to similar cases without ultrasound, with lower hemoglobin content in UAL suction.
[10] As practiced today, third-generation UAL has a low complication rate.
[11]
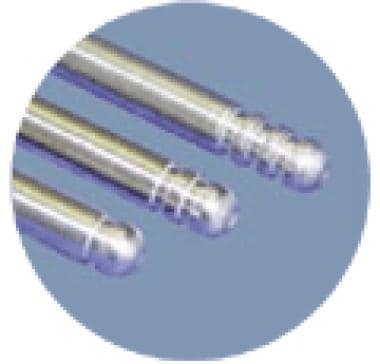
VASER detectors with grooves.
Continuous movement of the cannula is recommended to minimize the potential for focal, secondary thermal injury. While some practitioners have adopted a slow, deliberate style and others favor fast movement with high amplitude settings, the speed at which the cannula is advanced should be determined by the degree of resistance at a given energy level. Loss or resistance to cannula advancement is a strict endpoint because it indicates complete tissue emulsification.
Multifrequency (eg, pulsed versus continuous) has been suggested as a beneficial technical improvement,
[12] although the supporting data is largely subjective. Another application is for the treatment of multiple systemic liposuction.
[13] In this situation, the lipomas are not encapsulated, so the specific benefits of adding ultrasound also remain subjective.
There remains some debate as to whether UAL enhances skin contraction. Since this is a phenomenon that is difficult to measure objectively, claims that the indications for the use of UAL extend to high-volume cases or patients with loose skin have not been supported. Presumably, skin contraction will be stimulated by controlled thermal damage to dermal collagen. Modern techniques and technology have not developed so that this can be achieved safely and predictably.
The use of UAL for very large fat removal is also controversial. Since a moist environment is necessary for efficient conduction of acoustic energy into adipose tissue, injection of a wetting solution is required. The ratio of infused wetting solution to expected fat suction is 1:1.5-2, regardless of whether this results in tissue. Although it may be possible to achieve massive liposuction with minimal blood loss, the volumes of wetting solution required are associated with significant fluid shifts postoperatively.
The American Society of Plastic Surgeons (ASPS) recommends that outpatient lipoplasty be limited to 5000 mL of total suction, regardless of technique.
[14]
Complications
Early clinical series reported high rates of UAL-associated sera. These can be avoided by paying attention to technique, especially width adjustments and application duration. If seromas occur, they are usually treated with sequential suction and postoperative compression.
Skin burn is another complication that can be avoided by using skin protectors or cooling wraps. Some surgeons have found that skin pads are unnecessary since fluid oozes from the entry site and the cannula continues to move without putting pressure on the adjacent skin. A greater risk may be “end bumps” resulting from impaction of the tip of the cannula on the underlying skin surface, particularly with second-generation devices. Care must be taken to avoid skin ‘tenting’ by the tip of the cannula during ultrasound application.
A systematic approach is important, working either from the deep to the surface or vice versa. Superficial application of UAL may be associated with a higher risk of skin burns, seromas, and uneven skin contraction.
Perform final contouring after reaching an ultrasonic endpoint. This stage is done with standard cannulae and separate incisions can be used for “fine tuning” with microcannulas if needed. The overall end point for the lipoplasty procedure is determined by satisfactory contour and not by markers for discontinuing the ultrasound segment. Because of the extensive fragmentation of adipocytes in the emulsion, aspiration is not suitable for reimplantation.

